Wound dressing is a cornerstone of wound care management, serving as both a protective barrier and a therapeutic agent in the healing process. The appropriate choice of dressing not only accelerates wound closure but also reduces infection risk, maintains an optimal healing environment, and improves patient comfort. Advances in biomedical materials and clinical practice have led to a diverse range of dressings tailored to specific wound types, depths, exudate levels, and infection risks. Understanding the technical aspects of wound dressings is essential for healthcare professionals to optimize outcomes in acute and chronic wound management.
Core Functions of Wound Dressings
A wound dressing must fulfill multiple physiological and clinical functions simultaneously:
- Protection: Shields the wound from external mechanical trauma, microbial invasion, and environmental contaminants.
- Moisture Balance: Maintains an optimal moist environment to facilitate cell migration, angiogenesis, and granulation tissue formation, while preventing maceration of surrounding skin.
- Exudate Management: Absorbs excess fluid to prevent accumulation, which may delay healing or promote bacterial colonization.
- Gas Exchange: Permits oxygen diffusion to support cellular metabolism while allowing carbon dioxide and water vapor escape.
- Thermal Regulation: Provides insulation to maintain normothermic wound bed conditions, enhancing enzymatic activity and cellular proliferation.
- Atraumatic Removal: Minimizes tissue damage, pain, and disruption of new granulation tissue during dressing changes.
- Antimicrobial Action (optional): Incorporates agents (e.g., silver, iodine, honey) to suppress bacterial colonization in infected or high-risk wounds.
Classification of Wound Dressings
1. Traditional Dressings
- Gauze: Cotton-based, inexpensive, widely available. Primarily protective and absorptive, but can adhere to wound surfaces, causing trauma upon removal.
- Tulle dressings: Gauze impregnated with paraffin or medicated substances; reduce adherence but limited in moisture retention.
2. Modern Advanced Dressings
- Hydrocolloids: Occlusive dressings that form a gel upon contact with exudate, providing moisture retention and autolytic debridement. Ideal for low to moderate exudate wounds.
- Hydrogels: High water content, excellent for rehydrating necrotic tissue and promoting autolysis; unsuitable for heavily exudative wounds.
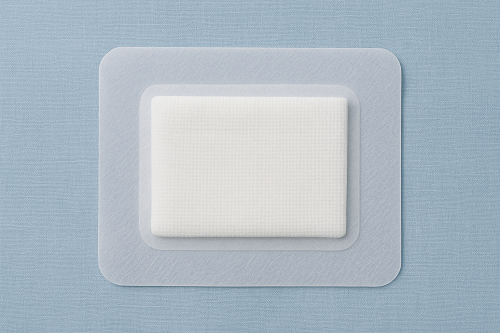
- Foam dressings: Highly absorptive, provide cushioning, and maintain a moist environment. Suitable for moderate to high exudate wounds.
- Alginates: Derived from seaweed, form hydrophilic gels upon contact with sodium-rich wound exudate. Highly absorptive and useful for bleeding wounds due to calcium content.
- Films (transparent polyurethane): Thin, semi-permeable to oxygen and water vapor but impermeable to bacteria. Used for superficial wounds with minimal exudate.
- Superabsorbents: Contain polymer cores with high fluid retention capacity; indicated in heavily exudating wounds.
3. Bioactive and Antimicrobial Dressings
- Silver dressings: Provide broad-spectrum antimicrobial activity by disrupting bacterial cell membranes and DNA.
- Iodine dressings (cadexomer iodine, povidone-iodine): Gradual release of iodine offers sustained antimicrobial effect without excessive cytotoxicity.
- Honey dressings (e.g., Manuka honey): Exhibit osmotic antibacterial action and anti-inflammatory properties.
- Chitosan-based dressings: Biodegradable and hemostatic, with inherent antimicrobial properties.
4. Next-Generation Smart Dressings
- pH-responsive dressings: Change color or properties depending on wound pH, signaling infection.
- Growth factor-loaded dressings: Deliver bioactive molecules to stimulate angiogenesis and fibroblast activity.
- Nanofiber scaffolds: Mimic extracellular matrix, enhancing cell migration and tissue regeneration.
- Electrical/photothermal dressings: Integrate microcurrents or photothermal elements to promote angiogenesis and combat biofilms.
Technical Issues in Wound Dressing Selection
1. Wound Assessment
- Type: surgical, traumatic, pressure ulcer, diabetic ulcer, venous ulcer.
- Depth and tissue involvement: superficial, partial-thickness, full-thickness.
- Presence of necrotic tissue or slough.
- Exudate level: none, low, moderate, high.
- Infection signs: odor, purulent discharge, erythema.
2. Moisture Balance Challenges
- Overly dry environment → scab formation and delayed epithelialization.
- Excessively wet environment → periwound maceration and bacterial overgrowth.
3. Biocompatibility and Cytotoxicity
- Dressings with chemical agents (e.g., silver, iodine) must balance antimicrobial efficacy with minimal cytotoxic effects on host cells.
4. Frequency of Dressing Change
- Highly exudative wounds may require daily changes, while occlusive dressings can remain for several days.
- Overly frequent changes disrupt healing; too infrequent may lead to bacterial proliferation.
5. Pain and Patient Comfort
- Atraumatic removal and soft-silicone interfaces are critical in managing fragile or chronic wounds.
- Dressing flexibility and conformability improve adherence to body contours.
6. Cost-Effectiveness
- Advanced dressings may be more expensive upfront but reduce overall costs through fewer dressing changes, lower infection rates, and faster healing.
Infection Control and Antimicrobial Resistance
Wound infection remains a major barrier to healing. While antimicrobial dressings reduce bioburden, their overuse may contribute to resistance or cytotoxicity.
Strategies include:
- Targeted antimicrobial dressing use only when infection is present or risk is high.
- Integration with systemic antibiotics for severe infections.
- Monitoring wound pH, exudate, and clinical signs to avoid unnecessary antimicrobial exposure.
Innovations and Future Directions
The future of wound dressing technology is moving toward personalized, intelligent systems that actively participate in wound healing.
- Biosensor-embedded dressings: Real-time monitoring of oxygen levels, exudate composition, and bacterial load.
- 3D-printed dressings: Custom-fitted to wound geometry with drug delivery capabilities.
- Regenerative biomaterials: Incorporating stem cells, exosomes, or tissue-engineered scaffolds to accelerate repair.
- Sustainable materials: Eco-friendly biopolymers to reduce medical waste.
Wound dressing has evolved from simple protective coverings to multifunctional, bioactive devices that play an integral role in wound healing. A successful wound management strategy requires accurate wound assessment, individualized dressing selection, and awareness of technical considerations such as moisture balance, infection control, and cost-effectiveness. With ongoing innovations in biomaterials and sensor technology, the next generation of wound dressings will not only protect and heal but also monitor and guide clinical decisions in real time.